By combining low intensity pulsed ultrasound (LIPUS) with lipid coated microbubbles, researchers at GW increased differentiation of human mesenchymal stem cells (hMSCs) into cartilage. Existing treatments for damaged cartilage include autografts, allografts, and total joint replacement. Autografts suffer from donor site morbidity and insufficient donor tissues, allografts have negative immune response, and total joint replacement patients may suffer from infection, implant loosening, osteolysis, or implant wear and tear. 3D printed constructs seeded with hMSCs offer potential to overcome the drawbacks of current techniques, but optimal cell growth and differentiation requires improved methods. Cartilage cells respond well to mechanical stresses induced by ultrasound treatment, and microbubbles are highly responsive to ultrasound treatment. Microbubbles oscillating due to ultrasound treatment can generate higher shear stresses on adjacent cells.
Differentiation of hMSCs to cartilage 3 weeks after seeding on hydrogel scaffolds greatly improved when combined with 0.5% lipid coated microbubbles and treated with LIPUS. Production of cartilage markers Glycosaminoglycan (GAG) and type II collagen increased by 17% and 78%, respectively. The 3D printed ultrasound and microbubble treated scaffolds may be implanted and subsequently treated with ultrasound. In vivo trials are planned.
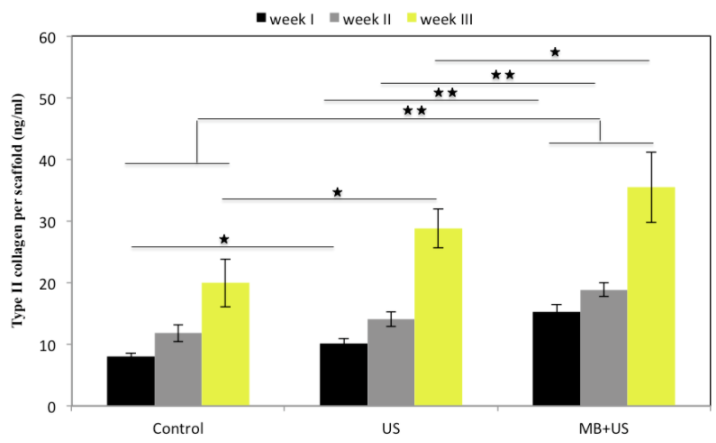
Figure: The amount of type II collagen per scaffold for weeks 1-3 in the control, the ultrasound treated scaffolds, and the ultrasound treated scaffold with microbubbles.
Applications:
- Living 3D printed implants to repair or replace damaged cartilage
- Treatment of implants prior to surgery to improve cell growth and differentiation
- Treatment of implants after surgery to improve cell growth and differentiation
Advantages:
- Increased differentiation of stem cells into cartilage tissue
- Adjustable scaffold size and shape